Antibiotic & Pesticide Resistance (Human Unintentional Artificial Selection) GRADED QUIZ
- Due May 4, 2020 at 11:59pm
- Points 20
- Questions 20
- Time Limit None
- Allowed Attempts 2
Instructions
Human Intervention – Unintentional Artificial Selection
As we have seen, Darwin’s theory of natural selection gets its name because it describes evolution of organisms based on selective pressures that occur naturally in the environment. However, many examples now exist where humans have either 1) unintentionally altered the environment to impact the evolution of new organisms, or 2) intentionally altered organisms through technology.
The appearance of humans on the evolutionary scene has lead to human manipulation of the environment, so as to accelerate the evolutionary process and unintentionally cause artificial selection. One example of this is the evolution of drug and chemical resistance in microbes, plants and animals. During the last half of the twentieth century, there has been an explosion in the appearance of agricultural and medical products to eliminate or control pests and pathogens. Examples include antibiotics to kill bacteria, pesticides to protect crops from insects, and chemotherapy drugs to destroy cancer cells. Yet, as we become better at fighting the enemy, we provide the selective pressure for evolution of new enemies who are even more effective in maintaining their stronghold. Overuse or misuse of products exacerbates the problem.
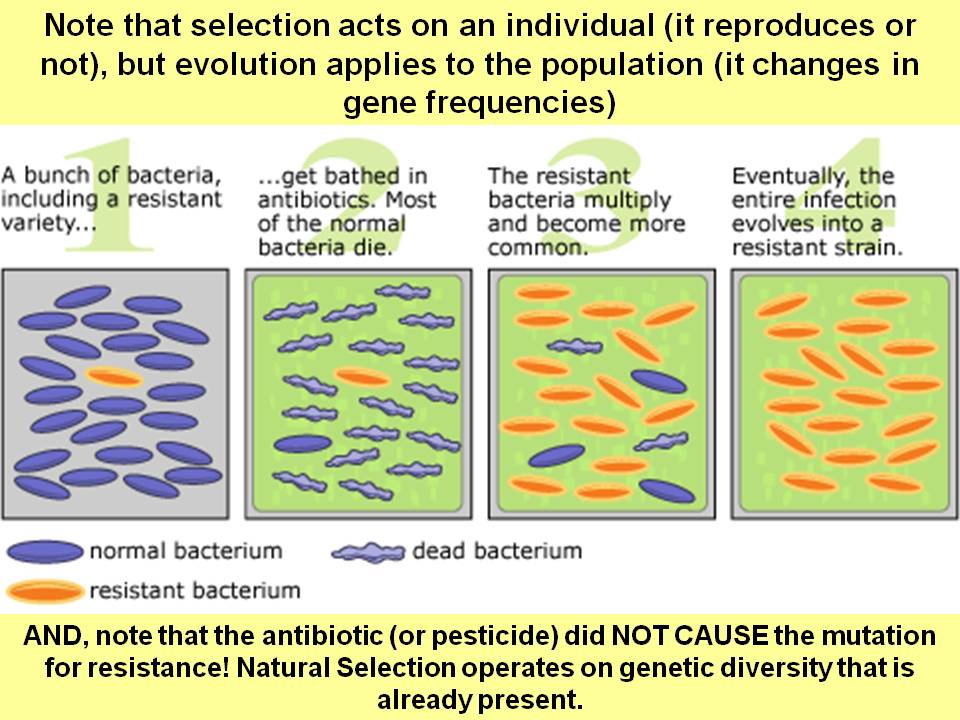
Consider the rapid rise in antibiotic-resistant bacteria. Both health professionals and patients share responsibility for allowing this problem to gradually surface. Although physicians know that antibiotics have no effect on viruses, for many years they succumbed to pressure from patients to give an easy cure for the common cold or the flu. Thus antibiotics were administered freely and inappropriately, to allow patients to feel that they were taking control of their sickness with a pill. In this way, strains of harmless (and in some cases beneficial) bacteria were attacked in the body, creating the niche for other hardier (and not so beneficial) bacterial strains to take their place. Even in patients with bacterial infections who were appropriately prescribed antibiotic treatment, many of those patients stopped taking the antibiotic as soon as they felt better, rather than taking the full course of antibiotic treatment. Once again, this practice destroys the weaker bacteria, while allowing the stronger individuals to remain, reproduce and increase their contribution to the bacterial gene pool. Thus, the genetic characteristics of bacteria have changed over time, favoring those who are more insidious at taking hold in the body and who do not respond to conventional antibiotics.